Reference Guide for Select Health First Choice Next Reference Guide for Select Health First Choice Next
Effective May 15, 2023, HNS' contract with Select Health includes Select Health First Choice Next.
The Select Health First Choice Next Quick Reference Guide provides important information regarding the First Choice Next plans, their members, claims, and Select Health policies. The information in this section is in addition to the HNS/Payor Polices.
This Quick Reference Guide contains the following information specific to First Choice Next.
General Information
Verifying Eligibility
Prior Authorization
Referral System
Copayments
First Choice Next ID Cards
Submitting Claims for First Choice Next Members
Corrected Claims
Claims Inquiries
Provider Relations
General Information
First Choice Next (Individual Plans On and Off Exchange)
Select Health First Choice Next is an HMO Benefit Program offered both on and off the Health Insurance Marketplace. It offers plans to individuals or families in select counties who do not have coverage through their employers, and do not qualify for Medicare or Medicaid.
Important Facts about First Choice Next plans:
- Benefits vary by member's plan level (Bronze, Silver, Gold).
- Preauthorization is required for First Choice Next members for many covered services, including but not limited to, Chiropractic Manipulative Treatment, so please verify benefits prior to rendering services to determine whether prior authorization is required.
- Effective 10/1/2023, when appropriate, Modifier AT is required to be appended to all Chiropractic Manipulative Treatment codes (98940, 98941, 98942, and 98943).
- Referral from PCP is NOT required.
- Claims must show First Choice Next in box 11c.
- Claims cannot be submitted electronically. (Submit all claims via paper using the CMS 1500 Claim Form.)
Please do not send claims directly to Select Health. All First Choice Next claims must be sent to HNS, and must be sent via paper claims.
If you have any questions about Select Health First Choice Next plans, please email your HNS Service Representative for assistance before calling Select Health. Your HNS Service Representative's email address is displayed on the provider dashboard on the secure section of the HNS website.
Back to Top
Verifying Eligibility
Always verify eligibility for each Select Health First Choice Next member.
To verify eligibility, refer to the telephone number on the member's identification card.
HNS' managed care partners list the HNS "participating providers" under the HNS master tax number/NPI in their systems and to obtain accurate information when verifying eligibility or benefits, you must use the HNS EIN and/or NPI.
Use the HNS EIN and/or HNS NPI number when verifying eligibility.
- The HNS EIN is 56-1971088.
- The HNS NPI number is 1093773392.
Back to Top
Prior Authorization
Prior authorization is required for many covered services including, but not limited to, Chiropractic Manipulative Treatment. As such, please verify benefits prior to rendering services to determine whether prior authorization is required and obtain prior authorization when required. If prior authorization is required, please also ensure that Box 23 on the Claim Form is completed with the applicable prior authorization number.
Back to Top
Referrals from PCPs
Referral from the member's primary care provider is not required.
Back to Top
Copayments
The copayment, if any, will vary by the plan in which the member is enrolled. Please refer to the member's ID card for the applicable specialist copay. If the member's plan has a specialist copayment, that copayment will be listed on the member's ID card and apply to services rendered by HNS providers.
Back to Top
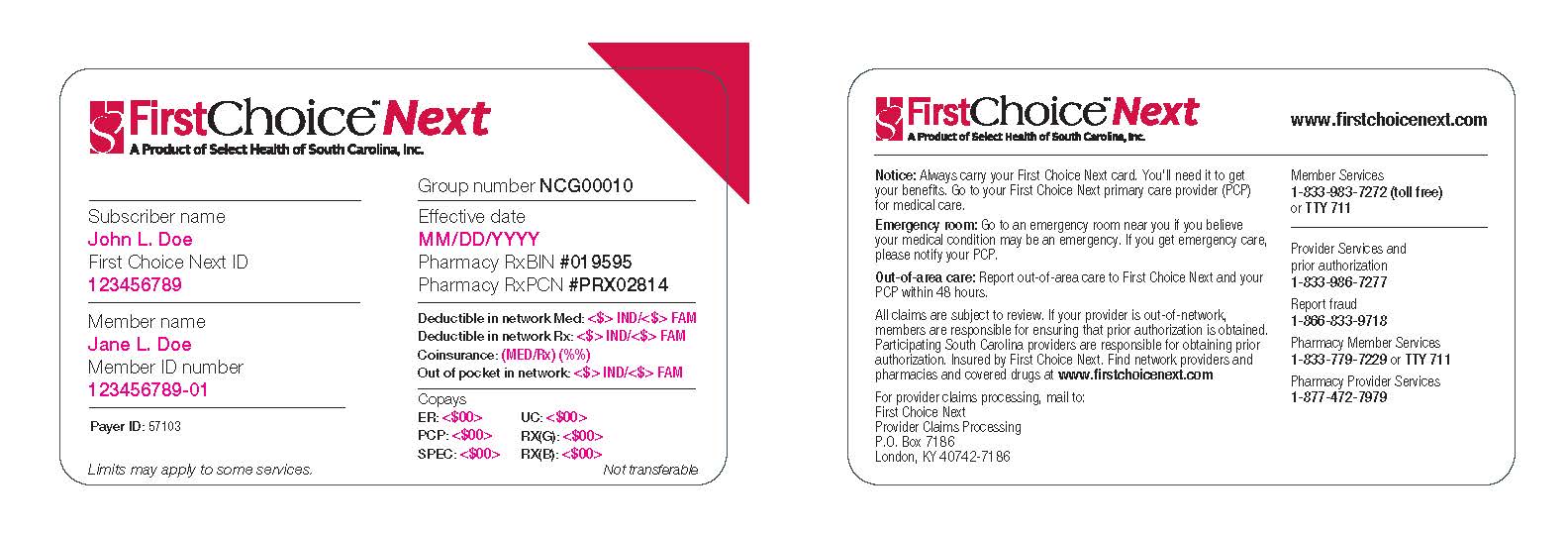
First Choice Next ID Cards
All First Choice Next claims must be submitted to HNS.
Members are easy to identify as their member ID card will clearly state "First Choice Next" A Product of Select Health of South Carolina, Inc.
Below is an example of the First Choice Next subscriber ID card. When a patient presents with this card, please remember that effective 5/15/2023, you are a participating provider with First Choice Next through your participation with HNS.
Please remember to obtain a copy of the front and back of the insurance card and maintain this in the member's health care record.
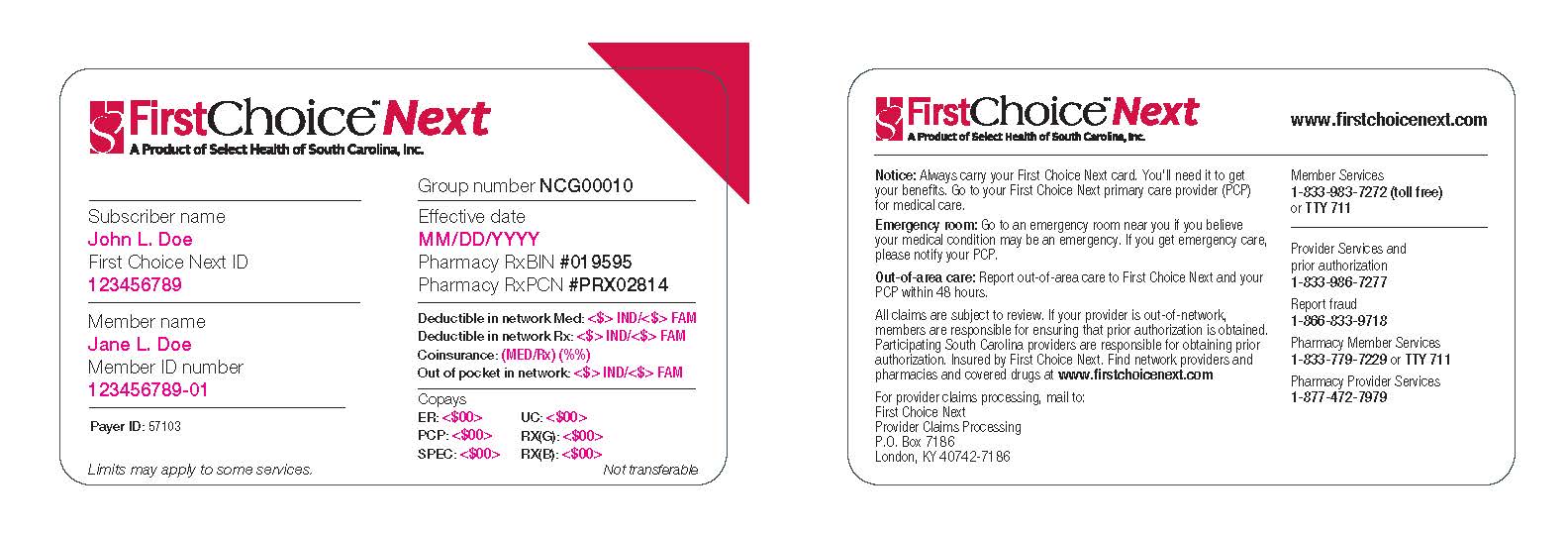
If you are uncertain about where to file the claim, please email your HNS
Service Representative a clear, legible copy of the member ID card and we will promptly respond back to you with an answer. Your HNS Service Representative's email address is displayed on the provider dashboard on the secure section of the HNS website.
Back to Top
Submitting Claims for First Choice Next Members
Please see an example of a First Choice Next claim (in the red vertical menu) and use this as a guide to ensure you correctly create the claim.
Claims must show First Choice Next in box 11c AND contain any required prior authorization number in box 23.
Effective 10/1/2023, Modifier AT is required to be appended to all Chiropractic Manipulative Treatment codes (98940, 98941, 98942, and 98943).
All Select Health First Choice Next claims must be sent to HNS. Please do not send claims directly to Select Health. Claims submitted directly to Select Health will process incorrectly and will have to be refiled.
Please ignore the claims billing address on the member ID card or any address given to you on the telephone when verifying eligibility and benefits. All Select Health First Choice Next claims must be sent to HNS.
How to File Claims:
All Select Health claims, even when filing claims electronically, must be identified as a Select Health claim in the address section at the top of the CMS 1500 claim form (HNS/Select Health is an acceptable format) using the example address below:
Example: HNS/Select Health
PO Box 2368
Cornelius, NC 28031
- At this time, First Choice Next claims cannot be submitted electronically to HNS.
- All claims for First Choice Next members must be sent to HNS as paper claims using the CMS 1500 claim form.
Required Information for Claims
- Claims must show First Choice Next in box 11c.
- Claims must contain any required prior authorization number in box 23.
Back to Top
Corrected Claims
When filing corrected claims to Select Health, claims must include the following:
- The claim must include the words "Corrected Claim" at the top of the claim.
- Box 22 (Resubmission code) - under this heading, you must include the #7 which indicates the claim is a corrected claim.
- Box 22 (Original ref. no.) - under this heading, instead of the reference number of the original claim, you must include the reference number shown on the most recently adjudicated claim. (Contact your HNS Service Representative if you cannot locate the reference number.)
- Box 23 (Prior Authorization) - under this heading, if applicable, you must include the original prior authorization number.
Please see an example of a corrected claim (in the red vertical menu) and use this as a guide to ensure you correctly create the claim.
Back to Top
Claims Inquiries
As previously noted, HNS' managed care partners list the HNS "participating providers" under the HNS master tax/NPI in their systems and to obtain accurate information when verifying eligibility or benefits, you must use the HNS EIN and/or NPI.
If you contact a payor directly (to obtain preauthorization, verify benefits or to trace a claim) and you are told that you are "out-of-network", use the HNS master federal tax number (EIN) and/or HNS' NPI instead of your own.
The HNS EIN is 56-1971088.
The HNS NPI number is 1093773392.
For tracing outstanding claims (after 60 days from your billing date), please email your HNS Service Representative and include the patient name, date of birth, member ID number and the dates of service in question. We will gladly trace the claim for you and will respond back to you within 3-5 business days.
Resubmit lost/missing claims through HNS.
Back to Top
Provider Relations
Questions relating to your participation in Select Health should be directed to your HNS Service Representative. Your HNS Service Representative's email address is displayed on the provider dashboard on the secure section of the HNS website.
Back to Top
|
 Health Network Solutions, Inc. (HNS) stands alone as the oldest and largest chiropractic network in the Southeast.
Health Network Solutions, Inc. (HNS) stands alone as the oldest and largest chiropractic network in the Southeast.